Introduction
People with long-term health conditions are often forced into low paid and insecure work – if they are able to work at all – with many struggling under the weight of debt.
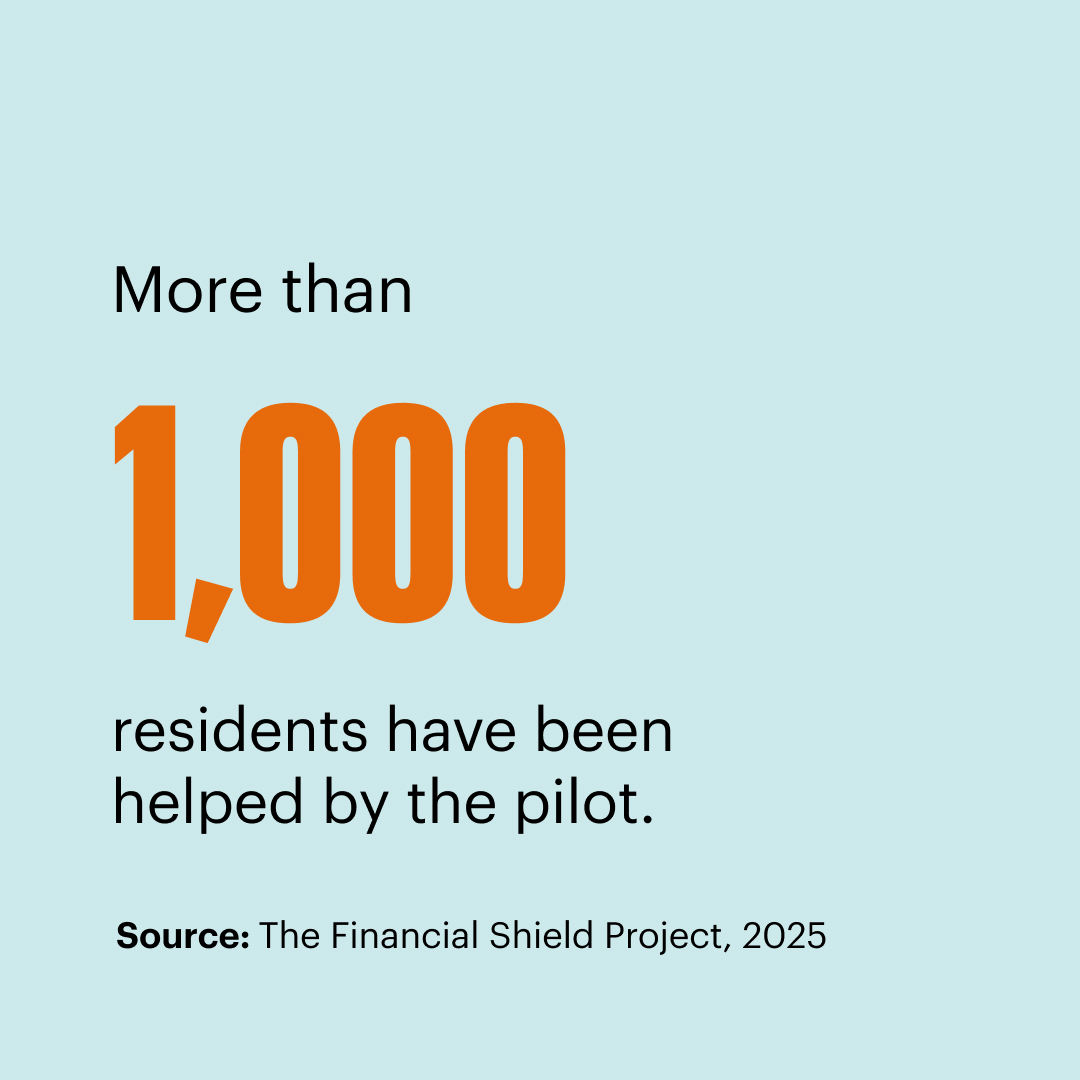
The Financial Shield project was developed to address this, tackling the two-way link between financial difficulties and poor health. This report demonstrates the impact that trusted, accessible, community-embedded support can have on both people’s financial circumstances and crucially their health.
About the Project
The Financial Shield pilot was launched in 2020, at the height of the pandemic, by Impact on Urban Health and the Centre for Responsible Credit. It set out to reduce the severe health and economic risks posed by Covid-19 in South-East London, focusing on working-age residents with, or at risk of, long-term health conditions.
A central feature is the use of Financial Support Link Workers (FSLWs), embedded within GP practices and primary care teams. These specialists provide tailored advice on benefits, debt, and financial management. Residents are referred by GPs and social prescribers, or can self-refer through a digital platform called Back on Track.
The partnership has brought together 34 GP practices, two councils, four housing associations, and local advice agencies such as Age UK Lambeth and Citizens Advice Southwark. This integrated model ensures trusted, high-quality advice is available where people already go for healthcare support.