Andrea’s story
Andrea is a 44-year-old and originally from Latin America. Her housing conditions were extremely bad, and they made her feel sick. Though the damp in her house made her asthma worse, better housing was unaffordable to her.
Financial foundations for adult health
Living one day at a time
Despite advances in public health practice and NHS provision, major health inequalities persist and are worsening for some people in the UK.
According to the Marmot Review and its 10-year follow-up, Fair Society Healthy Lives, health inequalities are exacerbated by economic and social issues, including financial health.
Many people with long-term health conditions and low incomes, including Luisa, struggle to properly access the right NHS services to get treatment for their conditions.
Luisa is a 28-year-old mother of two young children, aged one and four. She lives with depression and anxiety. Luisa and her husband, Tony, relocated from Portugal and have lived in the UK for the last six years.
Luisa used to work as a cleaner but became unemployed in 2018 when her depression and mental health deteriorated. It was really hard for Luisa to give up work because it had played an important role in her social life and in contributing to the household’s finances. After quitting her job, Luisa described what it felt like to live with constant anxiety:
In 2019, her health conditions improved a little, so she started looking for a job again. Unfortunately, the family had no help with childcare and Luisa’s one-year-old only had 15 hours of free nursery per week, which limited the type of work Luisa was able to look for.
She felt constrained because she found it difficult to combine childcare responsibilities with low-pay work. In August 2019, Luisa’s family needed money, so she managed to find an informal cleaning job again.
It wasn’t a lot of hours nor much income, but she was afraid that if she got a more formal job, her family would lose entitlement to Universal Credit, which was the most reliable income she had at the time.
Without support to navigate the benefits system, Luisa made some employment decisions based on flawed assumptions. Unfortunately, she had to quit the cleaning job in September since her anxiety worsened again.
Luisa isn’t alone in this situation. Many people with multiple health conditions have limited ‘mental bandwidth’ to make financial decisions, which significantly increase their stress levels and anxiety.
Luisa’s household income was not only low, but also varied from month to month (see graph below). Her husband Tony worked on a zero-hour contract, and his salary did not always cover essential expenses.
When they were strapped for cash, they mostly relied on loans and gifts from Tony’s mum and Luisa’s aunty. Sometimes, however, their family were not in a position to help, and Luisa and Tony asked others for loans, including Luisa’s boss.
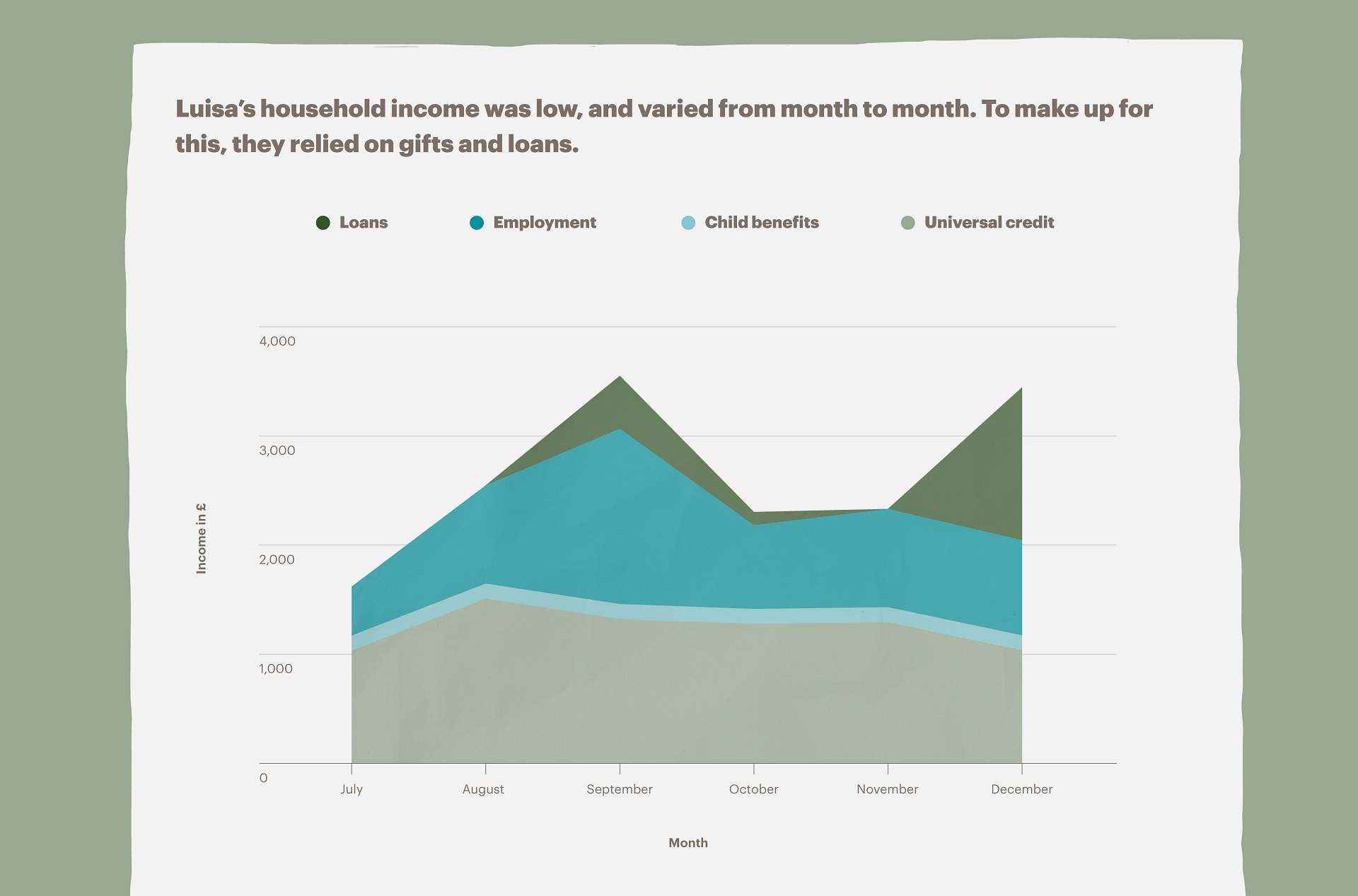
In December 2019, Luisa received a £1,400 loan from her boss. While she didn’t want to ask her boss for a loan, she urgently needed to rent a car while visiting her family in Portugal over the holidays.
Because Luisa and Tony couldn’t afford a car rental, they asked her boss for the loan. They were able to repay the loan within four days after receiving a delayed Universal Credit payment. Luisa found these informal debts were much easier to renegotiate and some, particularly with Tony’s mum, never had to be repaid.
Substantially less flexible were the £500 per month loans and arrears they had to repay. The first loan, with Brighthouse, was used to buy much-needed house appliances. The second loan was with the council.
When Luisa stopped working, they fell behind in their council tax payments, so they had to pay arrears twice every month. The third debt was with a mobile network provider and, finally, they had an overdraft with a commercial bank which they were trying to clear.
In addition, their household bills were usually around £200 per month. All these regular and important expenses left them with little room to pay for the rest of the things they needed, especially unexpected or high-cost expenses.
Luisa and Tony’s household income and expenditure were always very close, indicating that it was difficult for them to save (see graph below). During July, August, October and November 2019 when they did not receive any loans, they spent all the money that came into the household. This left them without any room to cope with emergency expenditures.
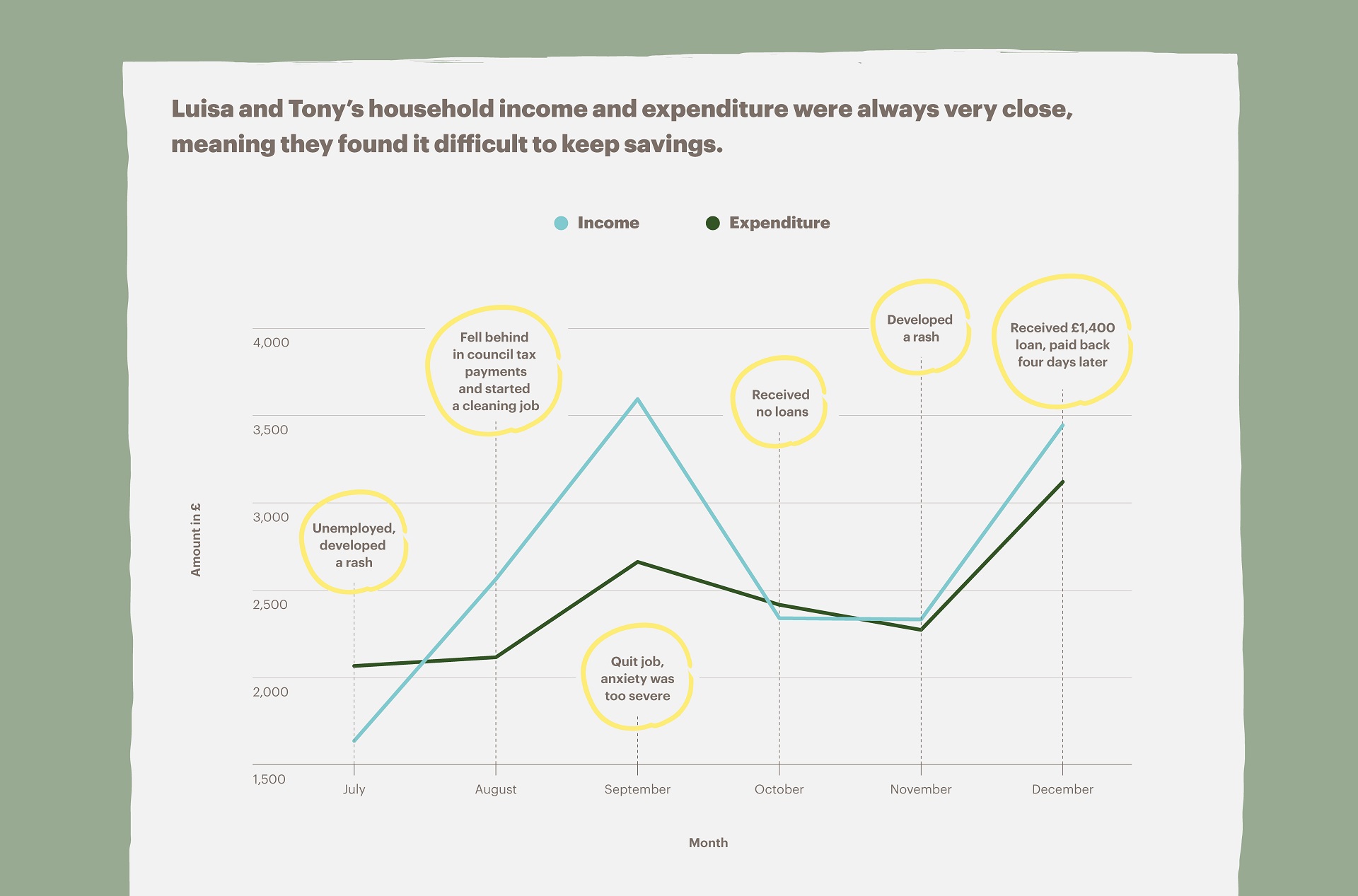
When reflecting on the connection between her depression and finances, Luisa explained that money uncertainty stresses her, noting that she even developed a rash on her skin. The rash came and went from July to December 2019, depending on her stress levels and income.
When Luisa went to the GP because of the rash, they told her that her mental issues and financial stress were manifesting themselves in her body through physical symptoms, but they did not offer any solutions beyond the diagnosis, such as a referral to social prescribing schemes to support with her financial needs.
Social prescribing is being rolled out nationally, in recognition of the connection between social factors, such as finances and housing, and health.
GPs can refer patients to Link Workers, who coordinate support for people around social needs, like Luisa’s financial difficulties. It’s important that GPs are aware of this and make use of it in cases like Luisa’s, so people aren’t turned away, like she was, with explanations, but not support.

Luisa preferred daily visits to small, nearby stores rather than less frequent grocery shopping at a bigger supermarket, even though she knew shopping at a bigger supermarket, where costs are lower, could save her money. “I prefer to pay this money every day” she explained. She added that she didn’t have the mental space to plan her meals in advance, so she sometimes went out for groceries several times a day.
When her depression and anxiety weren’t doing well, she bought compulsively. She described “the anxiety that wanting more than you need gives you”. Knowing that these compulsions weren’t helpful, she attempted to control herself since it not only had financial implications for the household but also brought tensions to her relationship with Tony.
By December 2019, Luisa was trying very hard to improve her life and the lives of her family members. Apart from receiving medical advice for her mental health and skin problems, she also sought help from community groups in the Borough—mostly parenting groups which she tried to attend regularly.
She also received free psychotherapy services from a local organisation that her GP referred her to during a period when it was hard for her to leave the house. Having a more direct link between expert financial advice and the health services would make advice more accessible to people with multiple long-term conditions, like Luisa, when they need it most.
By the end of 2019 Luisa was generally feeling better and making efforts to go out again, attend group meetings and mingle with others.
In January 2020, Luisa was determined to further her education and get a secure, meaningful job. To pay for her course she had to take out a £14,000 loan, which made the decision to go back to school extremely difficult because of the pressure she knew a new loan would put on her and Tony.
Her family’s uncertain household income, the state of her mental health and the lack of support with childcare were all additional factors Luisa had to weigh when considering the opportunities more education could provide.
From Luisa’s experience, these are the actions that organisations could make to protect the health of people like her:
Financial foundations for adult health
Andrea is a 44-year-old and originally from Latin America. Her housing conditions were extremely bad, and they made her feel sick. Though the damp in her house made her asthma worse, better housing was unaffordable to her.
Financial foundations for adult health
Daliya is a 27-year-old mother with multiple long-term health conditions living in South London. Her income fluctuated from month to month and her financial struggles had a huge impact on her mental health.
Financial foundations for adult health
Shannon is a 55-year-old single mother with four teenagers. Her precarious working conditions negatively impacted her health, especially when she couldn’t take paid time off work when she needed it.